Sleep is a fundamental requirement for a healthy body and mind. However, for many individuals, achieving a restful night’s sleep can seem like an elusive goal. Sleep disorders, like insomnia, narcolepsy, and sleep apnea, affect millions of people worldwide. Those who suffer from nightmare disorders might feel that sleep is anything but restful. Nightmares can cause intense feelings of fear, anxiety, and distress, leading to disrupted sleep patterns and daytime lethargy. The co-occurrence of sleep and nightmare disorders has become a topic of interest in recent years. In this article, we will explore the causes and treatments for these conditions and examine how people can improve their sleep quality and reduce the incidence of nightmares.
Contents
- The Basics of Sleep Disorders
- The Signs and Symptoms of Nightmare Disorders
- The Relationship Between Sleep Disorders and Nightmare Disorders
- Diagnosis and Treatment of Sleep and Nightmare Disorders
- Lifestyle Changes for Better Sleep and Fewer Nightmares
- Conclusion
-
Frequently Asked Questions
- What is the most common sleep disorder?
- Can sleep disorders lead to nightmare disorders?
- What are some common causes of nightmare disorders?
- Are medication interactions a potential cause of nightmare disorders?
- What is the impact of trauma on nightmare disorders?
- What are some diagnostic tests for sleep and nightmare disorders?
- What are some medications used to treat insomnia and sleep disorders?
- What is cognitive behavioral therapy (CBT), and how is it used to treat sleep and anxiety disorders?
- What lifestyle changes can improve sleep and reduce nightmares?
- Can nightmare disorders be cured?
- References
The Basics of Sleep Disorders
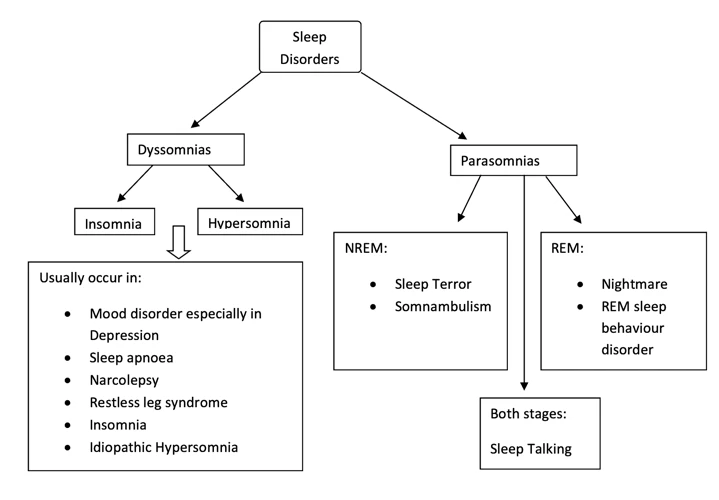
Sleep is an essential part of a healthy lifestyle, allowing the body to recharge and regenerate for the day ahead. However, many individuals struggle with sleep disorders that can interfere with their ability to achieve restful and restorative sleep. These disorders can take many forms, from difficulty falling or staying asleep to interrupted breathing during sleep. In this section, we will delve into the various types of sleep disorders, including insomnia, narcolepsy, sleep apnea, restless leg syndrome, and circadian rhythm disorders. Understanding the symptoms and root causes of these disorders is essential for proper diagnosis and effective treatment.
Insomnia
Insomnia is a common sleep disorder that affects many individuals. It is characterized by difficulty falling asleep, staying asleep, or both. The consequences of insomnia can be severe, as it can lead to fatigue, mood disturbances, and impairment in cognitive and physical functioning. There are several types of insomnia, which are listed in the table below:
| Type of Insomnia | Description |
|---|---|
| Acute Insomnia | A brief period of difficulty sleeping, usually lasting up to a few nights. |
| Chronic Insomnia | A long-term pattern of difficulty sleeping, typically defined as having trouble sleeping for at least three nights per week for three months or longer. |
| Primary Insomnia | Insomnia that is not attributed to another health condition, medication, or substance. |
| Secondary Insomnia | Insomnia that occurs as a result of another underlying condition, such as depression, anxiety, or chronic pain. |
| Onset Insomnia | Difficulty initiating sleep, often caused by anxiety or worry. |
| Maintenance Insomnia | Difficulty staying asleep, often characterized by waking up frequently during the night. |
Insomnia can be caused by a variety of factors, including stress, anxiety, depression, medical conditions, and certain medications. Treatment for insomnia often involves a combination of lifestyle changes and medication. It is important to consult with a healthcare professional if you are experiencing difficulty sleeping, as they can help to identify the underlying cause and develop a treatment plan.
Narcolepsy
Narcolepsy is a neurological disorder characterized by sudden, uncontrollable episodes of falling asleep during the day. It is a sleep disorder that affects the brain’s ability to regulate sleep-wake cycles.
People with narcolepsy often experience excessive daytime sleepiness and may feel the urge to take frequent naps throughout the day. The episodes of sleep can occur at any time, including during work or while driving, which can be dangerous.
Symptoms of narcolepsy
Along with excessive daytime sleepiness, people with narcolepsy may experience other symptoms, including:
| Cataplexy | A sudden loss of muscle tone, often triggered by strong emotions |
| Hallucinations | Vivid, often frightening, dream-like experiences that occur when falling asleep or waking up |
| Sleep paralysis | A temporary inability to move or speak when falling asleep or waking up |
| Fragmented nighttime sleep | Difficulty staying asleep and frequent awakenings during the night |
Causes of narcolepsy
The exact cause of narcolepsy is not fully understood, but it is believed to be a combination of genetic and environmental factors. Studies have found that people with narcolepsy have lower levels of the neurotransmitter hypocretin in their brains, which may contribute to the disorder.
Treatment for narcolepsy
There is currently no cure for narcolepsy, but medications can help manage the symptoms. Stimulants, such as modafinil and armodafinil, are often prescribed to help with excessive daytime sleepiness. Antidepressants, such as selective serotonin reuptake inhibitors (SSRIs), can help with cataplexy, hallucinations, and sleep paralysis.
Lifestyle changes, such as establishing regular sleep patterns and avoiding caffeine and alcohol, can also help improve symptoms of narcolepsy. It is important for individuals with narcolepsy to work closely with their healthcare providers to develop a treatment plan that works best for them.
Sleep Apnea
Sleep apnea can be a serious and potentially life-threatening sleep disorder that affects many people. It occurs when a person’s airway becomes partially or completely blocked during sleep, leading to interruptions in breathing that can last for several seconds or even minutes. There are two types of sleep apnea, obstructive sleep apnea (OSA) and central sleep apnea (CSA).
OSA is the more common type and occurs when the muscles in the throat relax and block the airway. This can lead to snoring, choking, or gasping during sleep as the person tries to catch their breath. CSA, on the other hand, is caused by a failure of the brain to send the proper signals to the muscles that control breathing. This can result in pauses in breathing, also known as apneas.
Sleep apnea can have serious consequences on a person’s overall health, including an increased risk of high blood pressure, heart disease, stroke, and diabetes. It can also lead to daytime fatigue, difficulty concentrating, and irritability.
Symptoms of sleep apnea can include:
| – Snoring | – Loud and constant snoring, especially with OSA |
| – Fatigue | – Daytime sleepiness, lack of energy, and difficulty concentrating |
| – Mood changes | – Irritability, depression, and anxiety |
| – Waking up to gasp or choke | – Especially with OSA |
| – Morning headaches | – Due to changes in oxygen levels during the night |
If you suspect that you or a loved one may have sleep apnea, a sleep study may be needed to diagnose the condition. Treatment options for sleep apnea typically include continuous positive airway pressure (CPAP) therapy, which uses a machine to deliver a constant stream of air through a mask to keep the airway open during sleep. Other treatments may include oral appliances that help reposition the jaw and tongue or surgery to remove excess tissue in the throat.
In addition to medical treatments, there are also lifestyle changes that can help alleviate sleep apnea symptoms. These may include weight loss, avoiding alcohol and sleeping pills, sleeping on one’s side instead of back, and quitting smoking. Making these changes can improve overall health and help decrease sleep apnea symptoms.
Restless Leg Syndrome
Restless Leg Syndrome, or RLS, is a neurological disorder that causes unpleasant sensations in the legs and the overwhelming urge to move them. This disorder affects an estimated 10% of adults and can significantly impact one’s quality of sleep. RLS symptoms typically worsen during periods of inactivity or at night, leading to insomnia and daytime fatigue.
Some common symptoms of RLS include:
- Uncomfortable sensations: an irresistible urge to move the legs due to tingling, crawling, creeping, or aching sensations
- Movement: temporary relief from these sensations by moving the legs or walking around
- Nocturnal aggravation: symptoms that become worse at night, resulting in difficulty falling asleep or staying asleep
- Discomfort relief: sensations that lessen with movement or by massaging the affected area
The causes of RLS are not entirely understood, but some theories suggest that certain factors such as iron deficiency, genetics, and other medical conditions like kidney disease, diabetes, or peripheral neuropathy could play a role. In some cases, RLS may be a side effect of medication.
Treatment for RLS typically involves addressing underlying medical conditions and a combination of medications such as dopamine agonists, anticonvulsants, and iron supplements. Additionally, making certain lifestyle changes, like regular exercise, avoiding caffeine and alcohol, and maintaining good sleep hygiene, can help reduce symptoms of RLS.
Consulting with a healthcare provider is essential for managing RLS symptoms and improving overall sleep quality.
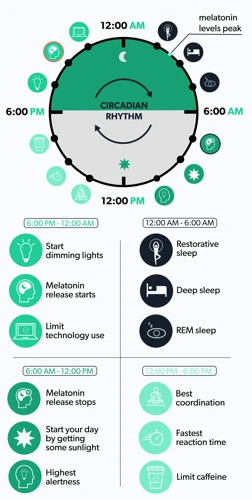
Circadian Rhythm Disorders
Circadian rhythm disorders refer to conditions in which an individual’s circadian rhythm is disrupted, causing disturbances in their sleep-wake cycle. The circadian rhythm is the natural 24-hour cycle that regulates our sleep and wakefulness. Disruptions in this rhythm can occur due to a variety of reasons, including work schedules, jet lag, and certain health conditions.
Types of Circadian Rhythm Disorders
There are several types of circadian rhythm disorders. These include:
| Type of Circadian Rhythm Disorder | Description |
|---|---|
| Delayed Sleep Phase Syndrome (DSPS) | A condition in which an individual has a hard time falling asleep until later in the night, and then has difficulty waking up in the morning. |
| Advanced Sleep Phase Syndrome (ASPS) | A condition in which an individual falls asleep earlier than normal and wakes up earlier than usual. |
| Non-24-Hour Sleep-Wake Disorder | A condition in which an individual’s sleep-wake cycle is longer than 24 hours, making it difficult to maintain a normal sleep schedule. |
| Shift Work Disorder | A condition that affects individuals who work non-traditional hours, causing disruptions to their sleep and wakefulness. |
Symptoms of Circadian Rhythm Disorders
Symptoms of circadian rhythm disorders may vary depending on the type of disorder an individual has. However, common symptoms include:
- Difficulty falling asleep or waking up at the desired times
- Feeling fatigued or sleepy during the day
- Difficulty concentrating and memory problems
- Mood disturbances, such as depression or irritability
Treatment for Circadian Rhythm Disorders
Treatment for circadian rhythm disorders may depend on the type of disorder an individual has and the severity of their symptoms. Treatments may include:
- Light therapy
- Chronotherapy
- Medications, such as melatonin or stimulants
- Cognitive behavioral therapy (CBT)
- Lifestyle changes, such as maintaining a regular sleep schedule and avoiding screens before bedtime
If you suspect that you have a circadian rhythm disorder, it’s important to speak with your healthcare provider, who can help you determine the best course of treatment for your symptoms.
The Signs and Symptoms of Nightmare Disorders
Nightmares are a common experience that many people have from time to time. However, for some individuals, nightmares can occur frequently and disrupt their sleep quality and overall well-being. When this happens, it is known as a nightmare disorder, which can have a significant impact on an individual’s mental and physical health. In this section, we will explore the signs and symptoms of nightmare disorders, including frequent nightmares, trauma-related nightmares, sleep terrors, and sleep paralysis. Understanding these symptoms can help individuals identify if they are experiencing a nightmare disorder and seek appropriate treatment.
Frequent Nightmares
Frequent nightmares refer to experiencing disruptive or frightening dreams multiple times a week or more. These nightmares can cause significant distress and affect a person’s daily life. Some common causes of frequent nightmares include:
- Stress and Anxiety: Experiencing ongoing stress and anxiety may lead to an increase in nightmares. This could be due to the brain processing the day’s events during REM sleep or due to the release of stress hormones during sleep.
- Medications and Substances: Certain medications and substances may increase the likelihood of nightmares, including antidepressants, beta-blockers, and alcohol.
- Sleep Disorders: Sleep disorders such as sleep apnea or narcolepsy may increase the likelihood of nightmares. Nightmares may also occur during withdrawal from certain sleep medications.
- Trauma: Trauma, specifically post-traumatic stress disorder (PTSD), can cause frequent nightmares related to the traumatic event. These nightmares may be vivid and disturbing, and can greatly affect a person’s quality of life.
It’s important to seek help if frequent nightmares are affecting your daily life. Treatment options may include medications, therapy, or lifestyle changes to improve sleep habits.
Trauma-related nightmares occur as a result of a person experiencing a traumatic event. These can include but are not limited to, sexual or physical assault, military combat, natural disasters, accidents, and the sudden death of a loved one. These nightmares can be intensely vivid and realistic, causing the individual to wake up feeling intense fear, panic, or distress. The content of these nightmares can vary, but they typically involve a re-experiencing of the traumatic event.
Characteristics of Trauma-Related Nightmares
Trauma-related nightmares are typically more intense and vivid than regular nightmares. They often involve realistic and graphic details of the traumatic event that the person experienced, causing them to relive the experience in their sleep. These nightmares may also occur more frequently if the person is experiencing high levels of stress or anxiety.
Treatment for Trauma-Related Nightmares
Treating trauma-related nightmares often requires a trauma-based therapy approach. This typically involves helping the individual process the traumatic event and develop coping mechanisms to manage the distressing thoughts and emotions associated with it. Two common types of trauma-based therapy for nightmares are Cognitive Processing Therapy (CPT) and Prolonged Exposure Therapy (PE).
CPT involves helping the individual challenge and change their thoughts and beliefs about the traumatic event. This therapy helps individuals to reframe the event and view it in a more positive and accepting way, reducing the emotional intensity of the memories and lowering the likelihood of experiencing recurring nightmares.
PE focuses on exposure to the traumatic event and the associated emotions and memories. This therapy aims to desensitize the individual to the trauma by gradually exposing them to the memories in a safe and controlled environment, allowing them to regain control over their thoughts and emotions.
In addition to therapy, certain medications, such as prazosin, may be prescribed to reduce the frequency and intensity of nightmares.
Sleep Terrors
Sleep terrors, also known as night terrors, are a type of parasomnia that usually occurs during the deepest stage of non-REM sleep. During a sleep terror episode, a person might suddenly sit up in bed, scream, and appear to be in a state of panic or fear, often sweating and breathing heavily. Despite appearing awake, a person experiencing a sleep terror is actually asleep and unaware of their surroundings.
Sleep terrors are different from nightmares, which occur during REM sleep and are usually remembered upon waking. While a person may not remember a sleep terror episode, they may feel groggy or agitated upon waking, and the lack of restful sleep can impact their daily functioning.
| Common characteristics of sleep terrors | Who is at risk? |
|---|---|
| Age: Sleep terrors are most common in children between the ages of 3 and 12, although they can occur in adults as well. | Genetics: A family history of sleep disorders may increase the risk of sleep terrors. |
| Frequency: Sleep terrors may occur multiple times a night or every few nights, usually during the first few hours of sleep. | Medical conditions: Certain conditions such as fever, asthma or sleep apnea may increase the risk of sleep terrors. |
| Duration: A sleep terror episode usually lasts between 1 and 10 minutes, and the person will usually fall back asleep afterwards. | Stress: High levels of stress or anxiety may trigger or worsen sleep terrors. |
There is no known cure for sleep terrors, but they can be managed through lifestyle changes and, in severe cases, medication. A consistent sleep schedule and reducing stress and anxiety can help prevent sleep terrors, as can creating a calm and relaxing sleep environment. If sleep terrors are interfering with daily life or causing injuries, medication may be prescribed to help reduce their frequency or severity. It’s important to work with a healthcare provider to determine the best course of action for managing sleep terrors.
Sleep Paralysis
Sleep paralysis is a type of nightmare disorder where a person experiences the inability to move or speak while waking up or falling asleep. In this state, the individual is conscious, but their muscles are paralyzed. While the exact cause of sleep paralysis is unknown, it is believed to be related to disrupted REM sleep.
The following are some symptoms of sleep paralysis:
- Feeling unable to move or speak when waking up or falling asleep
- Having a sensation of pressure on the chest or a feeling of suffocation
- Experiencing hallucinations, which is the perception of something that is not actually there, such as seeing or hearing things that are not present
- Feeling intense fear or anxiety
It is important to note that sleep paralysis is often associated with other sleep disorders such as:
- Narcolepsy
- Insomnia
- Sleep apnea
Some other factors that may contribute to an increased risk of sleep paralysis include:
- Irregular sleep patterns or lack of sleep
- Stress and anxiety
- Substance abuse
- Family history of sleep paralysis
Diagnosis and treatment for sleep paralysis:
If you have symptoms of sleep paralysis, it is important to speak with a healthcare provider for proper diagnosis and treatment. It may also be helpful to keep a sleep diary to track when and how often episodes occur. Treatment for sleep paralysis may include improving overall sleep hygiene, medication for underlying sleep disorders, and therapy to manage anxiety and stress.
Lifestyle changes that may help reduce symptoms include:
- Practicing good sleep hygiene by going to bed and waking up at the same time every day
- Avoiding caffeine, alcohol, and nicotine before bed
- Reducing stress through exercise, meditation, or therapy
- Sleeping in a cool, dark, and quiet environment
Sleep paralysis can be a frightening and uncomfortable experience. However, with proper diagnosis and treatment, it can be managed effectively.
The Relationship Between Sleep Disorders and Nightmare Disorders

The interplay between sleep disorders and nightmare disorders is a perplexing topic in the field of sleep medicine. In fact, the relationship between these two conditions is a complex web, with many factors contributing to their co-occurrence. Understanding this relationship is crucial in providing effective diagnostic and treatment strategies. The interactions between sleep disorders and nightmare disorders involve common causes, such as anxiety and depression, medication interactions, and the impact of trauma. In this section, we delve deeper into the intricate connection between sleep disorders and nightmare disorders.
Common Causes
When investigating the co-occurrence of sleep and nightmare disorders, it is important to consider the common causes that contribute to both types of disorders. Here are some of the most significant causes:
| Common Causes |
| Stress and anxiety |
| Depression |
| Medication interactions |
| Substance abuse |
| Trauma or PTSD |
| Irregular sleep schedule |
Stress and anxiety are the most common causes of both sleep and nightmare disorders. When you are under stress or experiencing anxiety, it can be difficult to fall asleep and stay asleep through the night. This often leads to insomnia, which in turn increases your chances of experiencing nightmares. Additionally, anxiety and stress can make the content of your dreams more distressing, leading to more frequent and intense nightmares.
Depression is another major cause of both sleep and nightmare disorders. Depression can lead to insomnia, hypersomnia or other sleep disturbances, which can in turn lead to nightmares. Additionally, depression can cause negative thoughts and emotions that can manifest in your dreams as nightmares.
Medication interactions can also cause sleep and nightmare disorders. Some medications you may be taking for other health conditions can affect your sleep cycles or cause nightmares as a side effect. It is essential to talk with your healthcare provider about any potential side effects of the medications you are taking.
Substance abuse can also contribute to both sleep and nightmare disorders. For example, the use of drugs or alcohol can disrupt your sleep patterns and lead to vivid and often disturbing dreams.
When an individual has experienced trauma or PTSD, they are at a greater risk of developing both sleep and nightmare disorders. Trauma can cause hyperarousal and anxiety, making it difficult to fall or stay asleep, and may lead to nightmares that are often related to the traumatic event.
Finally, an irregular sleep schedule can contribute to both types of disorders. Irregular sleep can mean you are not getting enough sleep, which can cause various sleep disorders. It is therefore essential to maintain a consistent sleep schedule, even on weekends or during vacations. Regular sleep helps regulate your body’s natural cycles and promote restful sleep.
The Role of Anxiety and Depression
Anxiety and depression often play a significant role in the occurrence and persistence of both sleep and nightmare disorders. Chronic or severe psychological distress can lead to difficulty falling asleep, maintaining a normal sleep cycle, and even cause a number of unpleasant physical symptoms such as irritability, fatigue, and changes in appetite. Individuals with anxiety and depression often experience heightened levels of emotional and physical arousal, which can increase the likelihood of both vivid dreams and nightmares.
The following are ways in which anxiety and depression can contribute to sleep and nightmare disorders:
- Hyperarousal: Anxiety and depression can cause hyperarousal, which results in the body being unable to relax and slip into a healthy sleep cycle. This can trigger night terrors or consistent nightmares which can contribute to sleep difficulties.
- Stress: Chronic stress can lead to both insomnia and nightmares. When the body is under stress, cortisol levels rise, leading to physical and mental stress. Chronic stress can result in heightened frequency and intensity of nightmares.
- Negative Thought Patterns: Individuals with anxiety and depression sometimes have negative thought patterns that can prevent them from sleeping well. This may result in frequent awakenings throughout the night in combination with nightmares.
- Medication Side Effects: Some medications prescribed for anxiety and depression, such as selective serotonin reuptake inhibitors (SSRIs), can cause vivid dreams and nightmares. People taking these medications may require treatment for both their psychological distress and the sleep problems caused by medication side effects.
- Daytime Fatigue: People with anxiety and depression may feel fatigued during the day due to disrupted sleep cycles or repeated nightmares, which can affect overall quality of life.
It is important to diagnose and treat any underlying anxiety and depression to effectively manage sleep and nightmare disorders. Treatment options for anxiety and depression include medication, therapy, mindfulness and relaxation techniques, and lifestyle changes. Proper treatment can often lead to a significant improvement in sleep quality and a reduction in the frequency and intensity of nightmares.
Medication Interactions
Taking certain medications can contribute to both sleep and nightmare disorders. Some medications can affect sleep patterns or cause side effects that disrupt sleep, leading to insomnia or other sleep disorders. Others can interfere with the normal function of the brain and increase the likelihood of experiencing nightmares.
Here are some common types of medications that can potentially interact with sleep and cause nightmares:
- Antidepressants: Some antidepressant medications can increase the likelihood of experiencing nightmares, particularly selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors (SNRIs), and tricyclic antidepressants (TCAs).
- Beta-blockers: These medications are commonly used to treat high blood pressure and anxiety disorders, but they can also interfere with sleep patterns and cause nightmares in some people.
- Narcotics: Opioid painkillers and other narcotics can affect sleep by causing drowsiness or disrupting normal REM sleep cycles, which can contribute to the development of nightmares.
- Stimulants: Stimulant medications like Ritalin or Adderall, which are commonly used to treat attention deficit hyperactivity disorder (ADHD), can make it difficult to fall asleep and stay asleep, which can lead to insomnia and worsen existing sleep disorders.
It is important for individuals who are taking any of these or other medications to talk to their healthcare provider about the potential side effects and interactions with sleep. Your healthcare provider may be able to adjust your dosage or switch you to a different medication that is less likely to cause sleep or nightmare disruptions. It is important not to stop taking any medications without first consulting with your healthcare provider.
The Impact of Trauma
Experiencing trauma can have a significant impact on an individual’s sleep, potentially leading to nightmare disorders. Trauma can be defined as a deeply distressing or disturbing experience, often involving physical harm or the threat of physical harm.
Dysregulation of the Stress Response: Trauma can lead to dysregulation of the body’s stress response, which can cause difficulties with falling asleep or staying asleep. This can result in insomnia or other sleep disorders, which may increase the risk of developing nightmare disorders.
Re-experiencing Traumatic Events: Individuals who have experienced trauma may also have flashbacks or intrusive thoughts that can disrupt sleep and lead to nightmares. Trauma-related nightmares may occur frequently, even years after the initial traumatic event occurred.
Hyperarousal: Trauma can also lead to hyperarousal, which involves being easily startled or experiencing a heightened state of awareness. This can make it difficult to fall asleep, stay asleep, or return to sleep after a nightmare.
Co-Occurrence of PTSD and Nightmare Disorders: Posttraumatic Stress Disorder (PTSD) often co-occurs with nightmare disorders. In fact, frequent and distressing nightmares are one of the diagnostic criteria for PTSD.
Interference with Treatment: Trauma-related nightmares may also interfere with treatment for sleep and nightmare disorders. For example, individuals with PTSD may be hesitant to participate in exposure therapy, which is a commonly used treatment for nightmare disorders, because it involves confronting and processing traumatic memories.
The impact of trauma on an individual’s sleep cannot be underestimated. It is important to consider the role of trauma in the development and treatment of sleep and nightmare disorders, and to incorporate trauma-informed care in the management of these conditions.
Diagnosis and Treatment of Sleep and Nightmare Disorders
When it comes to addressing sleep and nightmare disorders, accurate diagnosis and effective treatment are critical. To achieve this, various diagnostic tests can provide helpful insights into underlying issues. In some cases, medication may be necessary to manage symptoms and promote restful sleep. Other treatments, such as cognitive behavioral therapy and trauma-based therapy, can also be highly effective. Additionally, lifestyle changes such as establishing a regular sleep schedule and creating a calm sleeping environment can contribute to better sleep and fewer nightmares. Let’s explore in detail the different aspects of diagnosing and treating sleep and nightmare disorders.
Diagnostic Tests
When it comes to diagnosing sleep and nightmare disorders, a number of different diagnostic tests may be utilized to determine the root cause of the issue. These tests can help healthcare providers determine the most appropriate treatment options for each individual patient.
Some of the most common diagnostic tests for sleep and nightmare disorders include:
- Polysomnography (PSG): This test is typically used to diagnose sleep apnea, as well as other sleep-related breathing disorders. It involves sleeping in a sleep lab while sensors are attached to the body to monitor things like heart rate, brain waves, and oxygen levels.
- Multiple Sleep Latency Test (MSLT): Primarily used to diagnose narcolepsy, this test involves taking several naps throughout the day, during which time brain activity and other physiological markers are monitored.
- Actigraphy: While not a diagnostic test in and of itself, actigraphy involves wearing a device that tracks movement and sleep patterns. This can be useful in diagnosing circadian rhythm disorders.
- Imaging Tests: In some cases, healthcare providers may use imaging tests such as magnetic resonance imaging (MRI) or computerized tomography (CT) scans to look for physical abnormalities that could be contributing to sleep or nightmare disorders.
These diagnostic tests, along with a thorough medical history and physical exam, can give healthcare providers a better understanding of the underlying causes of sleep and nightmare disorders. With this information, they can create a personalized treatment plan that takes into account the specific needs of each patient.
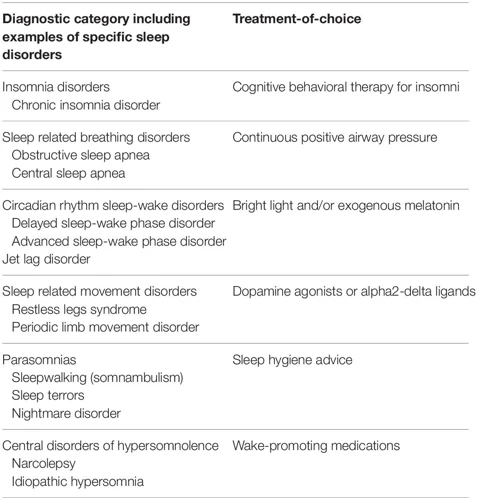
Medications for Insomnia and Sleep Disorders
There are several medications available to help treat insomnia and sleep disorders. These medications work to help regulate and promote healthy sleep patterns. Here are some examples of these medications:
| Medication | Function |
|---|---|
| Benzodiazepines (e.g., Valium, Xanax) | Helps relax muscles, reduce anxiety, and promote sleep |
| Non-Benzodiazepine Hypnotics (e.g., Ambien, Lunesta) | Works on the same receptors as benzodiazepines, but with less muscle relaxant effects |
| Antidepressants (e.g., Trazodone, Doxepin) | Can help regulate sleep patterns and improve mood |
| Antihistamines (e.g., Benadryl) | Helps alleviate allergies and promote drowsiness |
| Melatonin | A hormone that regulates sleep cycles, taken in supplement form to promote sleep |
It’s important to note that medication should not be the only form of treatment for sleep disorders. In many cases, medications can have side effects or can become habit-forming. It’s always best to discuss any potential medication use with a healthcare provider before starting a new regimen. Additionally, lifestyle changes and therapy can also be effective in treating sleep disorders.
Cognitive Behavioral Therapy for Insomnia and Anxiety
Cognitive Behavioral Therapy (CBT) is a form of therapy that has been shown to be effective in treating both insomnia and anxiety. CBT is typically done over several weekly sessions and is designed to help individuals understand and change the thoughts and behaviors that contribute to their sleep and anxiety problems.
The basics of CBT for insomnia
CBT for insomnia typically involves several techniques, including:
| Technique | Description |
|---|---|
| Sleep hygiene education | Teaching individuals about good sleep practices, such as establishing a regular sleep schedule and avoiding stimulating activities before bedtime. |
| Sleep restriction | Limits the amount of time spent in bed to only the amount of time spent sleeping. This helps to strengthen the association between the bed and sleep. |
| Stimulus control | Helps individuals associate the bed with sleep by only using the bed for sleep and sex. |
The basics of CBT for anxiety
CBT for anxiety typically involves several techniques, including:
| Technique | Description |
|---|---|
| Cognitive restructuring | Assisting individuals in changing negative thought patterns that contribute to their anxiety. |
| Exposure therapy | Gradually exposing individuals to situations that typically provoke anxiety, with the goal of reducing the intensity of the anxiety over time. |
| Relaxation training | Teaching individuals various relaxation techniques to help manage their anxiety, such as deep breathing exercises and progressive muscle relaxation. |
The benefits of CBT for insomnia and anxiety
CBT for insomnia and anxiety has been shown to have lasting benefits, even after therapy has ended. This is because CBT focuses on changing the underlying behaviors and thought patterns that contribute to insomnia and anxiety, rather than just treating the symptoms. Additionally, CBT is a non-invasive form of therapy that does not require medication, which can be appealing to individuals who prefer a more natural approach to treatment.
Trauma-Based Therapy for Nightmare Disorders
Trauma-based therapy can be an effective treatment for nightmare disorders that stem from past traumatic experiences. This form of therapy helps individuals process and cope with the trauma, which can ultimately lead to a decrease in the frequency and severity of their nightmares.
One type of trauma-based therapy is called Eye Movement Desensitization and Reprocessing (EMDR). During an EMDR session, the therapist guides the individual through a series of eye movements while they recall the traumatic memory. This process can help desensitize the individual to the memory, allowing them to process and reframe the experience in a more positive or neutral way.
Another type of trauma-based therapy is Cognitive Processing Therapy (CPT). CPT focuses on identifying and challenging unhelpful beliefs or thoughts related to the traumatic event, such as feelings of guilt or blame. The therapist works with the individual to reframe these thoughts and develop a more adaptive coping strategy.
A third type of trauma-based therapy is Prolonged Exposure (PE) Therapy. This form of therapy involves gradually exposing the individual to reminders of the traumatic event in a safe and controlled environment. Through this process, the individual can learn to confront and process their emotions related to the trauma, which can lead to a reduction in nightmares.
It is important to note that trauma-based therapy can be challenging and emotionally intense, and may not be appropriate for everyone. It is important to work with a qualified therapist who specializes in trauma to determine the best course of treatment for each individual.
Lifestyle Changes for Better Sleep and Fewer Nightmares
As we have seen, sleep and nightmare disorders can have a significant impact on our physical and mental health. While medical and therapeutic interventions can be beneficial, lifestyle changes can also play a crucial role in improving the quality and quantity of our sleep and reducing the frequency and intensity of our nightmares. In this section, we will explore some effective lifestyle changes that can promote better sleep and help prevent nightmares. By incorporating these strategies into our daily routine, we can take an active role in optimizing our sleep and overall well-being.
Establishing a Sleep Schedule
One key lifestyle change that can help improve both sleep and nightmare disorders is establishing a consistent sleep schedule. This means going to bed and waking up at the same times each day, even on weekends and holidays.
To establish a sleep schedule, it may be helpful to create a table to track your bedtime and wake-up times. Here is an example table:
| Day of the week | Bedtime | Wake-up time |
|---|---|---|
| Monday | 10:00pm | 6:00am |
| Tuesday | 10:00pm | 6:00am |
| Wednesday | 10:00pm | 6:00am |
| Thursday | 10:00pm | 6:00am |
| Friday | 10:00pm | 6:00am |
| Saturday | 11:00pm | 7:00am |
| Sunday | 11:00pm | 7:00am |
By sticking to a consistent sleep schedule, you can help regulate your body’s natural sleep-wake cycle, making it easier to fall asleep and wake up each day. This can also reduce the frequency and severity of nightmares.
It’s important to note that establishing a consistent sleep schedule may take some time and practice. Be patient with yourself as you adjust to the new routine, and don’t be too hard on yourself if you slip up occasionally. Just try to get back on track as soon as possible.
In addition to establishing a sleep schedule, there are other lifestyle changes that can help improve sleep and reduce nightmares, such as reducing stress and anxiety, avoiding triggers for nightmares, and creating a sleep-conducive environment. By taking a holistic approach to sleep and nightmare disorders, you can improve your overall well-being and quality of life.
Reducing Stress and Anxiety
Stress and anxiety are common causes of sleep and nightmare disorders. It is crucial to take steps to reduce stress and anxiety to promote better sleep quality and fewer nightmares. Here are some effective strategies for reducing stress and anxiety:
- Exercise: Regular physical activity can help reduce stress and anxiety levels. It releases endorphins, which are natural mood boosters. Engaging in at least 30 minutes of moderate exercise per day is recommended for optimal benefits.
- Mindfulness practices: Practicing mindfulness, such as meditation or deep breathing exercises, can help reduce stress and anxiety. These practices help to calm the mind and relax the body, making it easier to fall asleep and stay asleep.
- Aromatherapy: Using essential oils, such as lavender or chamomile, can have a calming effect and promote relaxation. Adding a few drops of essential oil to a diffuser or taking a warm bath with essential oils is a great way to add a relaxing scent to your bedtime routine.
- Journaling: Writing down your thoughts and emotions can help reduce stress and anxiety levels. This can be done before bed to clear the mind and promote better sleep.
- Healthy diet: Eating a well-balanced diet with plenty of fruits, vegetables, lean protein, and whole grains can help reduce stress and anxiety levels. Avoiding caffeine, alcohol, and sugary foods before bed can also improve sleep quality.
- Social support: Spending time with loved ones and engaging in social activities can help reduce stress and provide emotional support. This can be especially helpful for individuals who have experienced trauma and need extra support.
Incorporating these strategies into your daily routine can help reduce stress and anxiety levels, leading to improved sleep quality and fewer nightmares. It is important to consult with a healthcare provider to determine the best course of treatment for your individual needs.
Avoiding Triggers for Nightmares
It is ideal to identify potential triggers for nightmares and avoid them whenever possible. Common triggers include stress, anxiety, trauma, medications, and certain foods.
To reduce the likelihood of experiencing nightmares, it is recommended to avoid consuming stimulants such as caffeine, nicotine, and alcohol before bed. Additionally, spicy or heavy meals should be avoided as they may cause discomfort or disrupted sleep.
Stress and anxiety are significant contributors to the development of nightmare disorders. Stress-reducing activities such as exercise, yoga, or meditation may help reduce the frequency and intensity of nightmares. It is also important to create a relaxing bedtime routine and stick to a consistent sleep schedule.
If trauma is the underlying cause of the nightmare disorder, it may be helpful to avoid anything that triggers memories of the traumatic event. Avoiding violent movies or TV shows and refraining from discussing traumatic experiences before bedtime can reduce the frequency and intensity of nightmares.
Prescription medications may also contribute to the development of nightmare disorders. It is recommended to speak with a healthcare professional and report any unusual or disturbing dreams experienced during medication use.
Identifying and avoiding triggers for nightmares can significantly impact the management and treatment of nightmare disorders. A healthy lifestyle, stress reduction techniques, and eliminating triggers can help reduce the frequency and intensity of nightmares.
| Triggers to Avoid | Recommendations |
|---|---|
| Stimulants (caffeine, nicotine, alcohol) | Avoid consuming before bedtime |
| Spicy or heavy meals | Avoid consuming before bedtime |
| Stress and anxiety | Reduce with exercise, yoga, or meditation |
| Violent movies or TV shows | Avoid before bedtime |
| Traumatic experiences | Avoid discussing before bedtime |
| Prescription medications | Speak with a healthcare professional |
Creating a Sleep-Conducive Environment
A sleep-conducive environment can help promote better sleep quality and reduce the frequency of nightmares. Here are some tips for creating an optimal sleeping space:
| Tip | Description |
|---|---|
| Keep the Room Cool | Aim for a temperature between 60 and 67°F (15.5 and 19.5°C), which can help promote sleepiness and prevent overheating. |
| Minimize Noise | Use earplugs or a white noise machine to block out external noises that could disrupt sleep. |
| Eliminate Light | Use blackout curtains, an eye mask, or other strategies to keep the room dark and promote melatonin production. |
| Choose Comfortable Bedding | Opt for comfortable pillows and blankets that suit your individual preferences and promote relaxation and comfort. |
| Limit Screen Time Before Bed | Avoid using electronic devices for at least an hour before bedtime, as the blue light can suppress melatonin production and make it harder to fall asleep. |
| Create a Relaxing Atmosphere | Use calming colors, comfortable furniture, and soft lighting to create a peaceful and relaxing atmosphere in the bedroom. |
By taking steps to create a sleep-conducive environment, individuals with sleep and nightmare disorders can set themselves up for long-term success in managing their symptoms and achieving better sleep quality.
Conclusion
In conclusion, the co-occurrence of sleep and nightmare disorders can be a complex issue with a variety of potential causes and contributing factors. The basics of sleep disorders, including insomnia, narcolepsy, sleep apnea, restless leg syndrome, and circadian rhythm disorders, can disrupt normal sleep patterns and increase the likelihood of experiencing nightmares. The signs and symptoms of nightmare disorders, such as frequent nightmares, trauma-related nightmares, sleep terrors, and sleep paralysis, can have a significant impact on overall well-being and quality of life.
The relationship between sleep disorders and nightmare disorders is not always clear cut, but common causes include anxiety and depression, medication interactions, and the impact of trauma. Proper diagnosis and treatment can help individuals manage their symptoms and improve their quality of sleep. Diagnostic tests, medications for insomnia and sleep disorders, cognitive behavioral therapy for insomnia and anxiety, and trauma-based therapy for nightmare disorders can all be effective treatment options.
Lifestyle changes can also play an important role in improving sleep and reducing nightmares. Establishing a sleep schedule, reducing stress and anxiety, avoiding triggers for nightmares, and creating a sleep-conducive environment can all contribute to better sleep hygiene.
Overall, the co-occurrence of sleep and nightmare disorders can be a challenging issue to address, but with the right diagnosis, treatment, and lifestyle changes, individuals can improve their sleep and overall well-being. It is important to seek professional help if you are experiencing frequent nightmares or disrupted sleep, as these issues can have a significant impact on both physical and mental health.
Frequently Asked Questions
What is the most common sleep disorder?
Insomnia is the most common sleep disorder, affecting up to 30% of adults at some point in their lives.
Can sleep disorders lead to nightmare disorders?
Yes, sleep disorders can contribute to the development of nightmare disorders or make existing nightmares worse.
What are some common causes of nightmare disorders?
Common causes of nightmare disorders include anxiety, depression, PTSD, and certain medications.
Are medication interactions a potential cause of nightmare disorders?
Yes, certain medications such as antidepressants and beta blockers can lead to vivid dreaming or nightmares.
What is the impact of trauma on nightmare disorders?
Trauma can be a significant factor in the development of nightmare disorders, particularly those related to PTSD.
What are some diagnostic tests for sleep and nightmare disorders?
Diagnostic tests for sleep and nightmare disorders include a polysomnogram (sleep study), multiple sleep latency test, and psychological evaluations.
What are some medications used to treat insomnia and sleep disorders?
Common medications prescribed for insomnia and sleep disorders include hypnotics, sedatives, and anti-anxiety medications.
What is cognitive behavioral therapy (CBT), and how is it used to treat sleep and anxiety disorders?
CBT is a form of talk therapy that helps patients identify and change negative thoughts and behaviors that may be contributing to their sleep or anxiety issues.
What lifestyle changes can improve sleep and reduce nightmares?
Lifestyle changes that may help improve sleep and reduce nightmares include establishing a regular sleep schedule, reducing stress and anxiety, and creating a relaxing sleep environment.
Can nightmare disorders be cured?
Nightmare disorders can be effectively managed and treated in most cases, but a complete cure is not always possible.