As we drift off to sleep or wake up in the morning, we may experience a strange and unsettling phenomenon known as sleep paralysis. During this state, we are unable to move our body or speak, and often feel a sense of fear or dread. Adding to the confusion, we may also experience vivid and realistic hallucinations that can be difficult to differentiate from reality. These hallucinations, known as hypnagogic and hypnopompic hallucinations, can be both frightening and fascinating. In this article, we will explore the intricacies of sleep paralysis and delve into the science behind these mysterious hallucinations.
Contents
- What is Sleep Paralysis?
- What are Hypnagogic and Hypnopompic Hallucinations?
- Why Do Hypnagogic and Hypnopompic Hallucinations Occur in Sleep Paralysis?
- How Can You Cope with Hypnagogic and Hypnopompic Hallucinations in Sleep Paralysis?
- Conclusion
-
Frequently Asked Questions
- What is the difference between hypnagogic and hypnopompic hallucinations?
- How common are hypnagogic and hypnopompic hallucinations?
- Are hypnagogic and hypnopompic hallucinations dangerous?
- Can sleep paralysis occur without hallucinations?
- Can stress or anxiety cause hypnagogic and hypnopompic hallucinations?
- Do certain medications increase the likelihood of experiencing hypnagogic and hypnopompic hallucinations?
- What is lucid dreaming and how is it related to hypnagogic and hypnopompic hallucinations?
- Can hypnagogic and hypnopompic hallucinations be prevented?
- What can I do during a hypnagogic or hypnopompic hallucination?
- Should I see a doctor if I experience recurring hypnagogic and hypnopompic hallucinations?
- References
What is Sleep Paralysis?
Have you ever woken up in the middle of the night, only to find that you can’t move? It’s a terrifying experience that leaves you feeling trapped and vulnerable. Your mind may be awake, but your body is completely paralyzed. This phenomenon is known as sleep paralysis, and it affects up to 8% of the population. In this section, we’ll explore the definition and symptoms of sleep paralysis, as well as its causes and potential treatments.
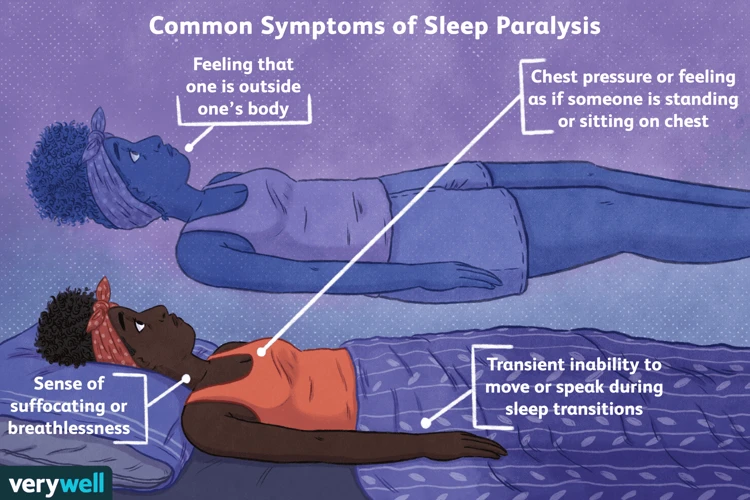
Definition and Symptoms
During sleep, the body goes through different stages, including Rapid Eye Movement (REM) and non-REM sleep. Sleep paralysis is a phenomenon that occurs during the state of REM sleep, in which the body becomes temporarily paralyzed, and the individual is unable to move or speak. This can be a frightening experience, especially if it is accompanied by hypnagogic or hypnopompic hallucinations.
Definition: Sleep paralysis is a condition in which a person experiences a temporary inability to move or speak while falling asleep or waking up.
Symptoms: The most common symptoms of sleep paralysis include:
- Being unable to move or speak
- Feeling a pressure or weight on the chest
- Hallucinations (visual, auditory, or tactile)
- A sense of impending doom or fear
- Difficulty breathing
These symptoms typically last a few seconds to a few minutes and can occur once or multiple times during the night. Sleep paralysis can be a one-time occurrence or a recurring issue for some individuals.
While sleep paralysis is not harmful in itself, it can be a symptom of an underlying sleep disorder, such as narcolepsy or sleep apnea. It can also be a sign of other health conditions, such as anxiety or depression. It is important to speak with a healthcare provider if sleep paralysis is a recurring issue.
In the next section, we will discuss the causes of sleep paralysis and how it relates to hypnagogic and hypnopompic hallucinations.
Causes
Various factors can lead to sleep paralysis. It can be caused by sleep deprivation, sleep schedule disruption, jet lag, or narcolepsy, which is a sleep disorder that causes excessive daytime sleepiness.
Additionally, stress and anxiety are also factors that can trigger sleep paralysis. The body’s response to stress and anxiety can alter the sleep-wake cycle, leading to disruptions in the normal pattern of REM sleep.
Furthermore, sleep-related breathing disorders such as sleep apnea can increase the likelihood of experiencing sleep paralysis. This is because these disorders can disrupt the normal flow of oxygen to the body and brain during sleep, which can lead to episodes of waking up during REM sleep.
Certain medications, such as antidepressants and antihistamines, and substance abuse, including alcohol and drug use, can also increase the risk of developing sleep paralysis.
It is important to note that sleep paralysis is not necessarily indicative of an underlying health condition or disorder, and it can occur in otherwise healthy individuals. However, if sleep paralysis regularly disrupts your sleep or causes distress, it is recommended to seek medical evaluation to rule out any underlying conditions.
The table below summarizes the common causes of sleep paralysis:
| Causes | Description |
|---|---|
| Sleep deprivation | Lack of adequate sleep |
| Sleep schedule disruption | Changes in the sleep-wake cycle, such as shift work or jet lag |
| Narcolepsy | A sleep disorder that causes daytime sleepiness |
| Stress and anxiety | Emotional and mental stress factors that affect sleep patterns |
| Sleep-related breathing disorders | Disorders such as sleep apnea that affect breathing during sleep |
| Medications | Certain medications like antidepressants and antihistamines |
| Substance abuse | Alcohol and drug use |
Treatment and Prevention
Sleep paralysis can be a frightening experience for those who suffer from it. Although there is no known cure for sleep paralysis, there are treatment and prevention techniques that can help alleviate the symptoms and reduce the frequency of episodes.
Treatment Techniques
| Technique | Description |
|---|---|
| Relaxation techniques | Deep breathing, meditation, and progressive muscle relaxation can help decrease anxiety and tension that may worsen sleep paralysis. |
| Sleep hygiene | Maintaining a consistent sleep schedule, avoiding caffeine and other substances that can disrupt sleep, and creating a comfortable sleep environment can help reduce the occurrence of sleep paralysis. |
| Cognitive-behavioral therapy (CBT) | CBT can help individuals change negative thought patterns and behaviors that may contribute to sleep paralysis. This therapy can also help reduce anxiety and improve overall sleep quality. |
Prevention Techniques
There are several steps individuals can take to prevent sleep paralysis from occurring:
| Technique | Description |
|---|---|
| Reduce stress | Stress can trigger sleep paralysis. Individuals can practice stress-reduction techniques such as exercise, meditation, or therapy to decrease stress levels. |
| Improve sleep habits | Establish a regular sleep schedule, limit caffeine and alcohol consumption, and create a comfortable sleep environment can help reduce the likelihood of sleep paralysis. |
| Address underlying conditions | Sleep disorders such as narcolepsy, obstructive sleep apnea, and restless leg syndrome can contribute to sleep paralysis. Treating these underlying conditions can help prevent episodes of sleep paralysis. |
By incorporating these treatment and prevention techniques into one’s lifestyle, individuals can manage the symptoms of sleep paralysis and ultimately lessen the impact it has on their quality of life.
What are Hypnagogic and Hypnopompic Hallucinations?
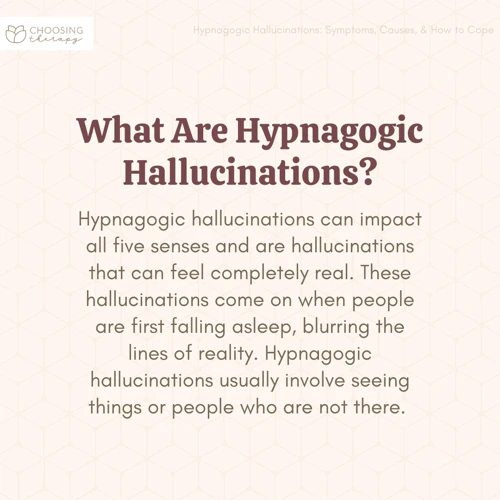
As we delve deeper into the world of sleep paralysis, we come across a term that might be unfamiliar to some: hypnagogic and hypnopompic hallucinations. These are vivid sensory experiences that occur during the transition into sleep (hypnagogic) or upon awakening (hypnopompic). These hallucinations can be frightening and confusing for those experiencing them, as they may feel like real-life experiences. In this section, we will explore the definitions and differences between hypnagogic and hypnopompic hallucinations and take a closer look at the common themes and examples that may arise during these experiences.
Definitions and Differences
Hypnagogic and hypnopompic hallucinations are two different types of hallucinations that can occur during sleep paralysis. While they share some similarities, they also have some important differences.
Hypnagogic hallucinations occur as a person is falling asleep. They can be vivid and often involve visual or sensory experiences. These experiences may include feeling like you are falling, seeing flashes of light, or hearing someone call your name.
Hypnopompic hallucinations occur as a person is waking up. They can also be vivid and may involve visual or sensory experiences. These experiences may include feeling like something is touching you or hearing someone whispering in your ear.
Comparison of Hypnagogic and Hypnopompic Hallucinations
| Hypnagogic Hallucinations | Hypnopompic Hallucinations |
| :— | :— |
| Occur as a person is falling asleep | Occur as a person is waking up |
| Vivid and often involve visual or sensory experiences | Vivid and may involve visual or sensory experiences |
| Can include feeling like you are falling, seeing flashes of light, or hearing someone call your name | Can include feeling like something is touching you or hearing someone whispering in your ear |
It is important to note that while hypnagogic and hypnopompic hallucinations are often described as occurring during sleep paralysis, they can also occur outside of sleep paralysis. Understanding the differences between these types of hallucinations can help individuals better identify and cope with any experiences they may have.
Common Themes and Examples
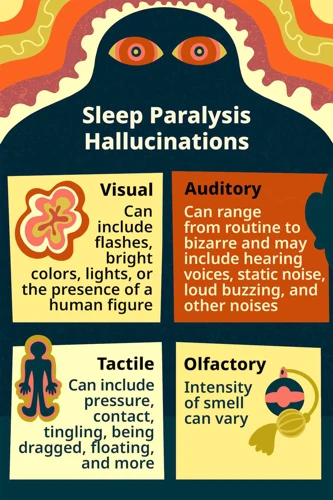
When it comes to hypnagogic and hypnopompic hallucinations, there are several common themes and examples that people tend to experience. These hallucinations can vary greatly from person to person, but below are some general examples that have been reported:
| Theme | Examples |
|---|---|
| Visual: | seeing people, animals, creatures, objects, or abstract patterns that aren’t actually there |
| Auditory: | hearing voices, music, or other sounds that aren’t actually present |
| Tactile: | feeling like someone or something is touching or holding you, even though there is no physical contact |
| Kinesthetic: | sensing movement or floating sensations, as if your body is moving without your control |
| Emotional: | feeling intense emotions, such as fear, happiness, or sadness, even though there is no obvious cause |
| Mixed: | a combination of any of the above hallucination types |
It’s worth noting that these themes and examples are not mutually exclusive and can occur simultaneously or in different combinations.
It’s also important to keep in mind that although these hallucinations can be vivid and frightening, they are not real and are simply a product of the brain’s activity during sleep paralysis.
Neuroscience of Hallucinations
Hallucinations, both hypnagogic and hypnopompic, are fascinating phenomena that have been studied extensively in the field of neuroscience. Research has provided insight into the neural mechanisms that underlie the experience of hallucinations.
One key finding is that hallucinations arise from a disruption in the normal functioning of the brain’s sensory systems. During normal perception, sensory information is processed and integrated in a coherent way, allowing us to make sense of our environment. However, during hallucinations, this integration is disrupted, leading to the generation of perceptual experiences that do not correspond to external reality.
Another important aspect of the neuroscience of hallucinations is the role of the brain’s default mode network (DMN). The DMN is a network of brain regions that are active when the brain is at rest and not engaged in any specific task. This network is thought to play a role in self-referential thinking and the generation of internal experiences, such as daydreaming.
Recent research has suggested that the DMN may also play a role in the generation of hallucinations. Specifically, it has been proposed that during sleep paralysis, the DMN becomes overactive, leading to the generation of internal experiences that are mistaken for external sensory experiences.
It has been suggested that the brain’s prefrontal cortex, which is involved in executive control and self-awareness, may also play a role in the generation of hallucinations. Specifically, it has been proposed that a disruption in the functioning of the prefrontal cortex may result in a breakdown in the ability to distinguish between internal and external experiences, leading to the generation of hallucinations.
Despite these recent insights, much remains unknown about the neuroscience of hallucinations, and further research is needed to fully understand the neural mechanisms that underlie these fascinating experiences.
The Neuroscience of Hallucinations
| Key Finding | Explanation |
|---|---|
| Disruption of sensory processing | Hallucinations arise from a disruption in the normal functioning of the brain’s sensory systems, leading to experiences that do not correspond to external reality. |
| Role of the default mode network | The brain’s default mode network (DMN) may play a role in the generation of hallucinations, as it is involved in self-referential thinking and the generation of internal experiences. |
| Role of the prefrontal cortex | The prefrontal cortex, which is involved in executive control and self-awareness, may also play a role in the generation of hallucinations, as a disruption in its functioning may result in a breakdown in the ability to distinguish between internal and external experiences. |
Why Do Hypnagogic and Hypnopompic Hallucinations Occur in Sleep Paralysis?
As we delve deeper into the world of sleep paralysis and hypnagogic/hypnopompic hallucinations, many of us may begin to question why these experiences occur in the first place. Is there a scientific explanation for the strange and often terrifying images and sensations we encounter while in this state? The answer, as it turns out, is complex and multifaceted, drawing on various factors such as the science of REM sleep, underlying stress and trauma, and the unique connection between hallucinations and lucid dreaming. With numerous theories and perspectives to explore, let us take a closer look at what may be behind our often bewildering experiences during sleep paralysis.
The Science of Sleep Paralysis and REM Sleep
The relationship between sleep paralysis and rapid eye movement (REM) sleep:
During normal sleep, our body cycles through different stages of sleep, including REM sleep, which is when we experience vivid dreams. During REM sleep, our body goes into a state of atonia, which is a natural paralysis that prevents us from acting out our dreams.
Sleep paralysis occurs when:
– Our body is in a state of atonia
– Our brain is awake and aware
This means that we are conscious during the paralysis, which leads to the sensation of being unable to move or speak.
Research has linked sleep paralysis to REM sleep:
– Studies have shown that sleep paralysis is more likely to occur during REM sleep or when transitioning in and out of REM sleep.
– This is why it is more common to experience sleep paralysis when sleeping on your back, as this position is associated with a higher likelihood of REM sleep.
Interestingly:
– It’s possible for individuals to experience sleep paralysis without realizing it, as it can occur during a brief window of wakefulness between sleep cycles.
– The sensation of being unable to move or speak during sleep paralysis may be caused by the brain’s misinterpretation of the body’s atonia as a physical restriction.
The relationship between sleep paralysis and REM sleep is complex and requires further research. However, the connection between the two highlights the importance of understanding the different stages of sleep and how they can impact our overall sleep experience.
The Role of Stress, Trauma, and Other Factors
Stress, trauma, and other factors can all contribute to the occurrence of hypnagogic and hypnopompic hallucinations in sleep paralysis. Stress, for example, can disrupt sleep patterns, leading to more frequent occurrences of sleep paralysis and the accompanying hallucinations. Additionally, individuals who suffer from anxiety or depression may be more likely to experience sleep paralysis and related hallucinations.
Trauma can also be a contributing factor. Those who have experienced trauma in their lives, such as abuse or a life-threatening event, may find themselves more susceptible to sleep paralysis and the associated hallucinations. In fact, studies have shown that individuals who have experienced trauma or have post-traumatic stress disorder (PTSD) are more likely to suffer from sleep disorders.
Other factors, such as a disrupted sleep schedule, alcohol or drug use, and certain medications, can also increase the likelihood of experiencing hypnagogic and hypnopompic hallucinations in sleep paralysis. It is important to note, however, that not all individuals who experience these factors will necessarily experience sleep paralysis or related hallucinations.
It is clear that various external and internal factors can play a role in the occurrence of sleep paralysis and the accompanying hallucinations. It is important for individuals who experience these symptoms to seek professional help, as there may be underlying mental health conditions that should be addressed.
The Connection Between Hallucinations and Lucid Dreaming
One of the fascinating connections between hallucinations and sleep is their link to lucid dreaming. Lucid dreaming refers to a state where a person is aware that they are dreaming and can even control their dreams to an extent. When a person enters a state of lucid dreaming, they may experience vivid hallucinations as they have greater control over their dream world.
In a sense, hypnagogic and hypnopompic hallucinations can be viewed as failed attempts at lucid dreaming. In a lucid dream, the dreamer is in full control, allowing them to turn their dreams into a rich sensory experience. In contrast, in a hypnagogic or hypnopompic hallucination, the dreamer is not fully in control, leading to a sense of fear or panic. These experiences may result from an attempt to maintain awareness during the transition to or from a dream state.
Researchers have found that certain techniques used to induce lucid dreaming, such as reality testing, can also help reduce the frequency of sleep paralysis and hypnagogic or hypnopompic hallucinations. One study found that teaching individuals lucid dreaming techniques, such as reality testing and keeping a dream journal, led to a reduction in the frequency of sleep paralysis and hypnagogic or hypnopompic hallucinations.
Despite their similarities, it is important to note that lucid dreaming and hypnagogic or hypnopompic hallucinations are distinct phenomena. Lucid dreaming is an intentional act performed by the dreamer, while hypnagogic and hypnopompic hallucinations are often unwanted experiences that occur naturally as part of the sleep cycle.
Below is a table comparing the key differences between lucid dreaming and hypnagogic/hypnopompic hallucinations.
| Lucid Dreaming | Hypnagogic/Hypnopompic Hallucinations | |
|---|---|---|
| Control | The dreamer is fully in control of their dream world. | The dreamer has limited control and may feel fear or panic. |
| Intention | The dreamer intentionally enters a state of lucid dreaming. | Hypnagogic/hypnopompic hallucinations occur naturally as part of the sleep cycle. |
| Outcome | A rich sensory experience where the dreamer can control and shape their dreams. | May result in fear or panic; often unwanted experiences. |
How Can You Cope with Hypnagogic and Hypnopompic Hallucinations in Sleep Paralysis?
Dealing with hypnagogic and hypnopompic hallucinations during sleep paralysis can be a terrifying and confusing experience. With these hallucinations often involving vivid and sometimes disturbing imagery or sensations, it’s no wonder many people struggle to cope with them. However, there are strategies and techniques that can help you manage these phenomena and reduce their impact on your sleep and daily life. In this section of the article, we’ll explore some self-help strategies and professional treatments that can make a difference.
Self-Help Strategies
Finding ways to cope with hypnagogic and hypnopompic hallucinations in sleep paralysis can be challenging, but there are self-help strategies that may be useful.
1. Relaxation techniques: Learning and practicing relaxation techniques can be beneficial in reducing stress and anxiety, which are contributing factors to sleep paralysis and hallucinations. Some techniques include deep breathing, progressive muscle relaxation, guided imagery, and mindfulness meditation.
2. Sleep hygiene: Maintaining good sleep hygiene can improve the quality of sleep and reduce the likelihood of experiencing sleep paralysis and hallucinations. This includes establishing a regular sleep routine, creating a comfortable sleep environment, avoiding stimulants such as caffeine and nicotine, and limiting the use of electronic devices before bedtime.
3. Cognitive-behavioral therapy: Cognitive-behavioral therapy can be helpful in identifying and changing negative thoughts and behaviors that may contribute to sleep paralysis and hallucinations. It can also provide coping strategies for dealing with anxiety and stress.
4. Lucid dreaming techniques: Practicing techniques for inducing lucid dreaming can be useful in turning a potentially negative experience into a positive one. It involves being aware that you are dreaming and being able to control the dream environment. This can be accomplished through reality checking, keeping a dream journal, and performing reality testing.
| Self-Help Strategies | Explanation |
|---|---|
| Relaxation techniques | Deep breathing, progressive muscle relaxation, guided imagery, and mindfulness meditation can help reduce stress and anxiety. |
| Sleep hygiene | Maintaining a regular sleep routine, creating a comfortable sleep environment, avoiding stimulants, and limiting electronics before bedtime can improve sleep quality. |
| Cognitive-behavioral therapy | Identifying and changing negative thoughts and behaviors through therapy can reduce anxiety and stress. |
| Lucid dreaming techniques | Practicing techniques for inducing lucid dreaming can allow for control of the dream environment and a more positive experience. |
It is important to note that self-help strategies may not work for everyone and seeking professional help may be necessary for more severe cases of sleep paralysis and hallucinations.
Professional Help and Medication
Professional Help and Medication
If self-help strategies are not sufficient in managing hypnagogic and hypnopompic hallucinations in sleep paralysis, it may be necessary to seek professional help. This can include seeing a therapist or counselor who specializes in sleep disorders or anxiety, or consulting with a sleep specialist who can conduct a sleep study to help diagnose and treat the underlying causes of sleep paralysis.
In some cases, medication may also be prescribed to help manage symptoms. Antidepressants such as selective serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants (TCAs) can be effective in treating sleep paralysis, as they can help regulate and balance brain chemicals involved in mood and sleep.
Additionally, medications such as benzodiazepines or other sedatives may be prescribed to help manage anxiety and promote relaxation before bedtime. It is important to discuss the potential benefits and risks of these medications with a healthcare provider, as they can have potential side effects and risks of dependency.
Seeking professional help and medication should only be considered after trying self-help strategies and lifestyle changes, and under the guidance and recommendation of a healthcare provider.
Conclusion
In conclusion, understanding hypnagogic and hypnopompic hallucinations in sleep paralysis is crucial for those who experience this phenomenon. While sleep paralysis can be a frightening and confusing experience, it is important to remember that it is a relatively common occurrence and can often be managed through self-help strategies or professional intervention.
Sleep paralysis is a result of the REM sleep cycle and can be caused by a range of factors including stress, trauma, and genetics. Hypnagogic and hypnopompic hallucinations, while often alarming, are a normal occurrence during these phases of sleep and are not indicative of any underlying mental health disorder.
It is vital to work with a healthcare professional to rule out any potential medical conditions that may be causing or exacerbating sleep paralysis. In addition, self-help strategies such as good sleep hygiene, stress reduction techniques, and relaxation exercises may help prevent or reduce the severity of sleep paralysis and associated hallucinations.
Professional intervention, including therapy and medication, may also be beneficial for individuals struggling with the emotional and psychological effects of sleep paralysis and hypnagogic and hypnopompic hallucinations.
Overall, education and awareness about sleep paralysis and hypnagogic and hypnopompic hallucinations can help reduce fear and anxiety associated with these experiences. By understanding the science behind these phenomena and implementing effective coping mechanisms, individuals can learn to manage and even overcome their sleep paralysis episodes.
Frequently Asked Questions
What is the difference between hypnagogic and hypnopompic hallucinations?
Hypnagogic hallucinations occur during the transition from wakefulness to sleep, while hypnopompic hallucinations occur during the transition from sleep to wakefulness.
How common are hypnagogic and hypnopompic hallucinations?
It is estimated that up to 25% of the population may experience these types of hallucinations at some point in their lives.
Are hypnagogic and hypnopompic hallucinations dangerous?
No, they are generally harmless and not a sign of any underlying medical condition.
Can sleep paralysis occur without hallucinations?
Yes, sleep paralysis can occur without hallucinations, but it is often accompanied by them.
Can stress or anxiety cause hypnagogic and hypnopompic hallucinations?
Yes, stress and anxiety can be trigger factors for these types of hallucinations.
Do certain medications increase the likelihood of experiencing hypnagogic and hypnopompic hallucinations?
Yes, some medications such as antidepressants and antipsychotics may increase the likelihood of experiencing these types of hallucinations.
Lucid dreaming is the ability to be aware that you are dreaming and control the content of your dreams. It is related to hypnagogic and hypnopompic hallucinations because both involve a blurred line between reality and imagination.
Can hypnagogic and hypnopompic hallucinations be prevented?
There is no surefire way to prevent these types of hallucinations, but maintaining good sleep habits and managing stress and anxiety may reduce the likelihood of experiencing them.
What can I do during a hypnagogic or hypnopompic hallucination?
Try to remain calm and recognize that it is not real. You can also try to move your fingers or toes to snap out of it.
Should I see a doctor if I experience recurring hypnagogic and hypnopompic hallucinations?
It may be a good idea to speak to a doctor or mental health professional if the hallucinations are causing significant distress or interfering with daily life.